Hypoglycaemia in Diabetes
In diabetes, hypoglycaemia for the most
part emerges as a result of pharmacologic treatment that causes blood glucose
levels to drop underneath the normal range. Whereas mild hypoglycaemia usually
resolves with incite ingestion of carbohydrates, more often reduced glucose
levels can impede cognitive function, and even threaten life.
Nocturnal
hypoglycaemia poses a specific challenge because the sleeping patient isn't in
a position to intervene and numerous episodes are asymptomatic. Repeated
exposure to nocturnal hypoglycaemia can limit counterregulatory mechanisms,
with possibly serious clinical consequences.
Hypoglycaemia
in diabetes typically happens as a result of therapeutic treatment,
particularly with insulin, glinides or sulfonylureas (SUs). Risk factors for
hypoglycaemia includes Aggressive treatment of glycaemia, HbA1C < 6.5%*
(except in youth), High glucose variability (in older adults), Long duration of
diabetes, Renal impairment, Duration of insulin therapy, Advanced age, Cognitive
impairment, Depression. In addition, insulin-related factors and specific
behaviours may influence the risk of nocturnal hypoglycaemia. Risk factors
includes: Missed meal, alcohol consumption, strenuous, dose of basal insulin
too high, too much rapid-acting insulin to correct high glucose, premix or
short-acting insulin before dinner, NPH insulin (isophane) in the evening.
An
episode of severe hypoglycaemia can lead to loss of consciousness, confusion and
seizures, with a concomitant increase in the risk of injuries, falls
and hospitalisation. Nocturnal hypoglycaemia will leads to disturbed sleep. Fear
of hypoglycaemia, in turn, can prevent adherence to medical treatment.
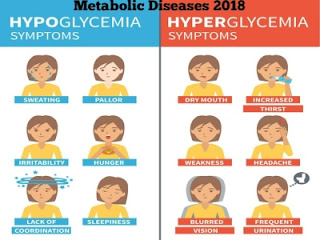
Impaired awareness of
hypoglycaemia (IAH) may be a
reduced ability to see the onset of hypoglycaemia. IAH emerges when rehashed
episodes of hypoglycaemia raise the glycaemic limit for symptom generation.
Symptoms that would make individuals mindful of approaching hypoglycaemia, such
as sweating or anxiety, no longer occur above the new limit. In addition, IAH
increases people’s dependence on others to treat their. Scrupulous avoidance of
hypoglycaemia can invert IAH, though in spite of the fact that this procedure
runs the chance of compromising glycaemic control.
Symptoms
of non-severe hypoglycaemia can be treated with 15 g fast-acting carbohydrate, such
as a few small sweets or sweetened drink or cup of milk, juice. Treatment is
additionally exhorted in asymptomatic patients with blood glucose in the alert
range of (63 to 70 mmol/L). If glucose levels stay low after 15 minutes, treatment
ought to be rehashed. In a conscious person, severe hypoglycaemia can be cured
in a comparative manner with 20 g fast-acting carbohydrates. On the off chance
that glucose remains low after 45 minutes, IV glucose can be considered if accessible.
In an unconscious person, hypoglycaemia is treated with glucagon or with IV
glucose.



Comments
Post a Comment