Diabetes Contributes to Cholesterol Metabolism
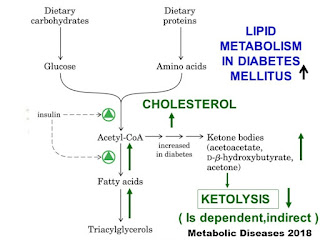
Diabetes mellitus is the most frequent endogenous cause of fat metabolism-disorder. Cholesterol metabolism is abnormal in diabetes. Total plasma cholesterol is increased, and more subtle indices of sterol homeostasis are also disturbed.
Hypertriglyceridemia in diabetes is due to an increase of chylomicrons, triglyceride-carrying lipoproteins and the very-low-density lipoproteins. In type I-diabetics the pathogenesis for hypertriglyceridemia is about decreased activity of the lipoproteinlipase, reduced chylomicron-clearance and the impeded degradation of VLDL. More often in non-insulin-dependent diabetics LDL-cholesterol-levels can be seen lifted and HDL-cholesterol-concentration decreased in correlation with the metabolic control. Primary hyperlipoproteinemia shows up regularly in diabetics, but this can be clarified with the association with obesity in type II-diabetics.
Dyslipidaemia in T2D is characterised by several strictly linked anomalies: increased fasting and postprandial triglycerides (TG), a noteworthy decrease in high‐density lipoprotein (HDL) cholesterol and an increment in smaller low‐density lipoprotein (LDL) and HDL particles. The increase in plasma TG is to a great extent clarified by the increased production of TG‐rich; large‐sized VLDL in particular. The insulin resistant liver fails to inhibit lipid attachment to pre‐VLDL molecules and synthesises larger‐sized VLDL at a more prominent rate. Large TG‐rich; VLDL enhances the transfer of core lipids between VLDL, LDL, and HDL with increased formation of smaller LDL and HDL.
Also, the elevated postprandial TG that is frequently shown in patients with T2D may be connected to insulin resistance. Therefore, the abatement of hyperglycaemia and insulin resistance ought to be one of the most treatment destinations to address dyslipidaemia in patients with diabetes.
Also HMG-CoA reductase, the rate-limiting enzyme in cholesterol synthesis, is elevated in small intestine, and diminished in liver in diabetic rats. These changes in reductase activity are due to hyperphagia (increased caloric and/or cholesterol intake), not to insulin deficiency alone, since diabetic rats confined to a typical food intake have normal reductase activity in small intestine and liver. It shows that increased input of dietary and newly synthesized cholesterol by the small intestine raises plasma cholesterol level and quells reductase activity in liver of chronically diabetic rats.
On the whole, diet plays a central role in the diabetic's cholesterol homeostasis. The hyperphagia of test diabetes increases net cholesterol intake and increased HMG-CoA reductase in a hypertrophic small intestine.



Comments
Post a Comment